Meningovascular Neurosyphilis in HIV Coinfected Patient
DOI:
https://doi.org/10.60591/crspmi.202Keywords:
Coinfection, HIV Infections, NeurosyphilisAbstract
Syphilis is a reemergent disease, with a prevalence increase
in Portugal of 14.8 times in five years (2016-2021). In people living with human immunodeficiency virus (HIV), syphilis appears in atypical and more severe forms, mainly in
patients with severe immunosuppression, being neurosyphilis one of the paradigms.
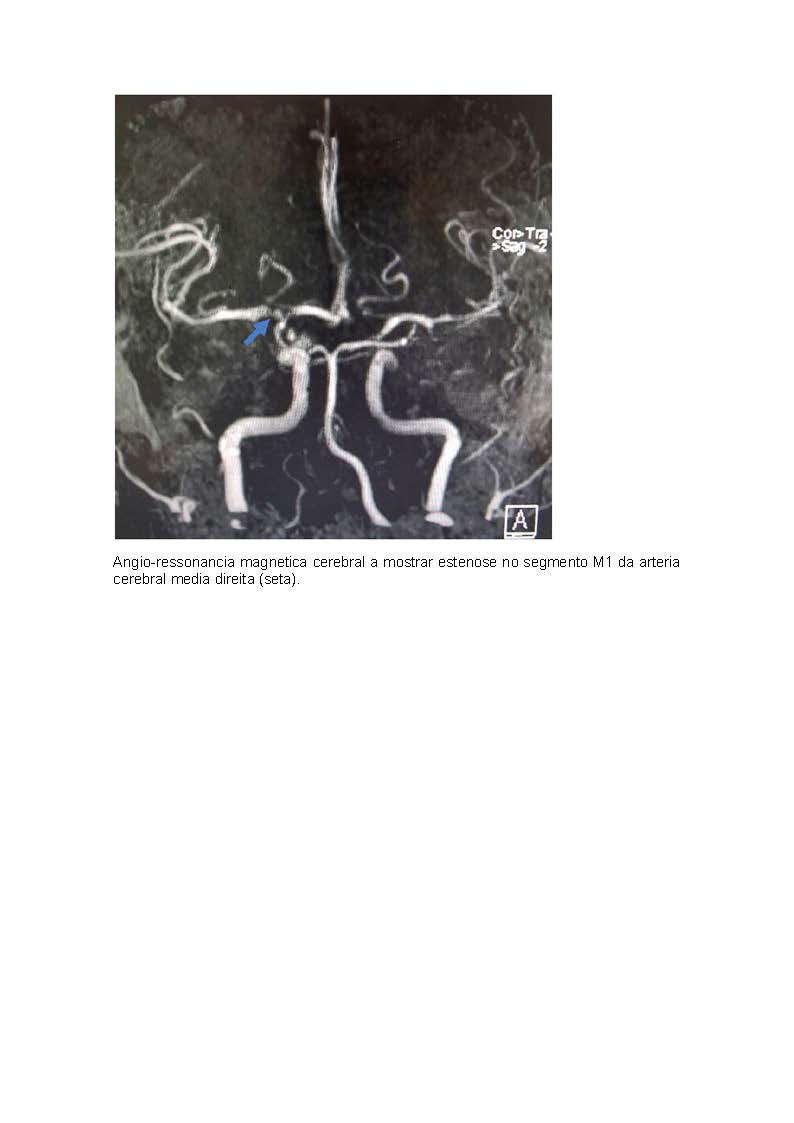
We present a clinical case of a 29 years-old man with
headache for one month, and sudden transitory speech impairment and left hemifacial paraesthesia. After clinical investigation, he was diagnosed with neurosyphilis in the form of syphilitic meningitis and meningovascular syphilis. In this episode, he was also diagnosed with HIV infection.
Neurosyphilis remains an important differential diagnose
of ischemic stroke. However, there are some specificities in
syphilis/HIV coinfection that deserve attention due to the increase in prevalence.
Downloads
References
Centers for Disease Control and Prevention. Sexually Transmitted Infections Treatment Guidelines, 2021 - Neurosyphilis, Ocular Syphilis, and Otosyphilis. Published online 2021. [consultado Jan 2023] Disponível em:https://www.cdc.gov/std/treatment-guidelines/neurosyphilis.htm
European Centre for Disease Prevention and Control. Surveillance Atlas of Infectious Diseases. [consultado Dez 2023]. Disponível em: https://atlas. ecdc.europa.eu/public/index.aspx
Hamill MM, Ghanem KG, Tuddenham S. State-of-the-Art Review: Neurosyphilis. Clin Infect Dis. 2023:ciad437. doi: 10.1093/cid/ciad437.
Hobbs E, Vera JH, Marks M, Barritt AW, Ridha BH, Lawrence D. Neurosyphilis in patients with HIV. Pract Neurol. 2018;18:211-8. doi: 10.1136/practneurol-2017-001754.
Ropper AH. Neurosyphilis. N Engl J Med. 2019;381:1358-63. doi: 10.1056/NEJMra1906228.
Tuddenham S, Ghanem KG. Neurosyphilis: Knowledge Gaps and Controversies. Sex Transm Dis. 2018;45:147-51. doi: 10.1097/
OLQ.0000000000000723
Zhou J, Zhang H, Tang K, Liu R, Li J. An Updated Review of Recent Advances in Neurosyphilis. Front Med. 2022;9:1-10. doi: 10.3389/
fmed.2022.800383
Ren M, Dashwood T, Walmsley S. The Intersection of HIV and Syphilis: Update on the Key Considerations in Testing and Management. Curr HIV/AIDS Rep. 2021;18:280-8. doi: 10.1007/s11904-021-00564-z
Ghanem KG. Evaluation and management of syphilis in the HIV-infected patient. Curr Infect Dis Rep. 2010;12:140-6. doi: 10.1007/s11908-010-0083-6
Janier M, Unemo M, Dupin N, Tiplica GS, Potocnik M, Patel R. 2020 European guideline on the management of syphilis. J Eur Acad Dermatol Venereol. 2021;35:574-88. doi: 10.1111/jdv.16946
Downloads
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Catarina Carreira da Costa, Sara Aleixo Cabrita, Pedro Gomes Santos, João Ferreira de Sousa, Motasem Shamasna

This work is licensed under a Creative Commons Attribution 4.0 International License.