Encephalopathy with Delirium and Generalized Tonic-Clonic Seizure in a Patient with Severe COVID-19
DOI:
https://doi.org/10.60591/crspmi.105Keywords:
COVID-19, Delirium, Encephalopathy, Organizing Pneumonia, SARS-CoV-2Abstract
Neurological manifestations of COVID-19, despite being far
less frequent than respiratory symptoms, are rising in importance, presenting a broad clinical spectrum.
The authors report the case of a 70-year-old man with
severe acute respiratory distress syndrome due to SARS-
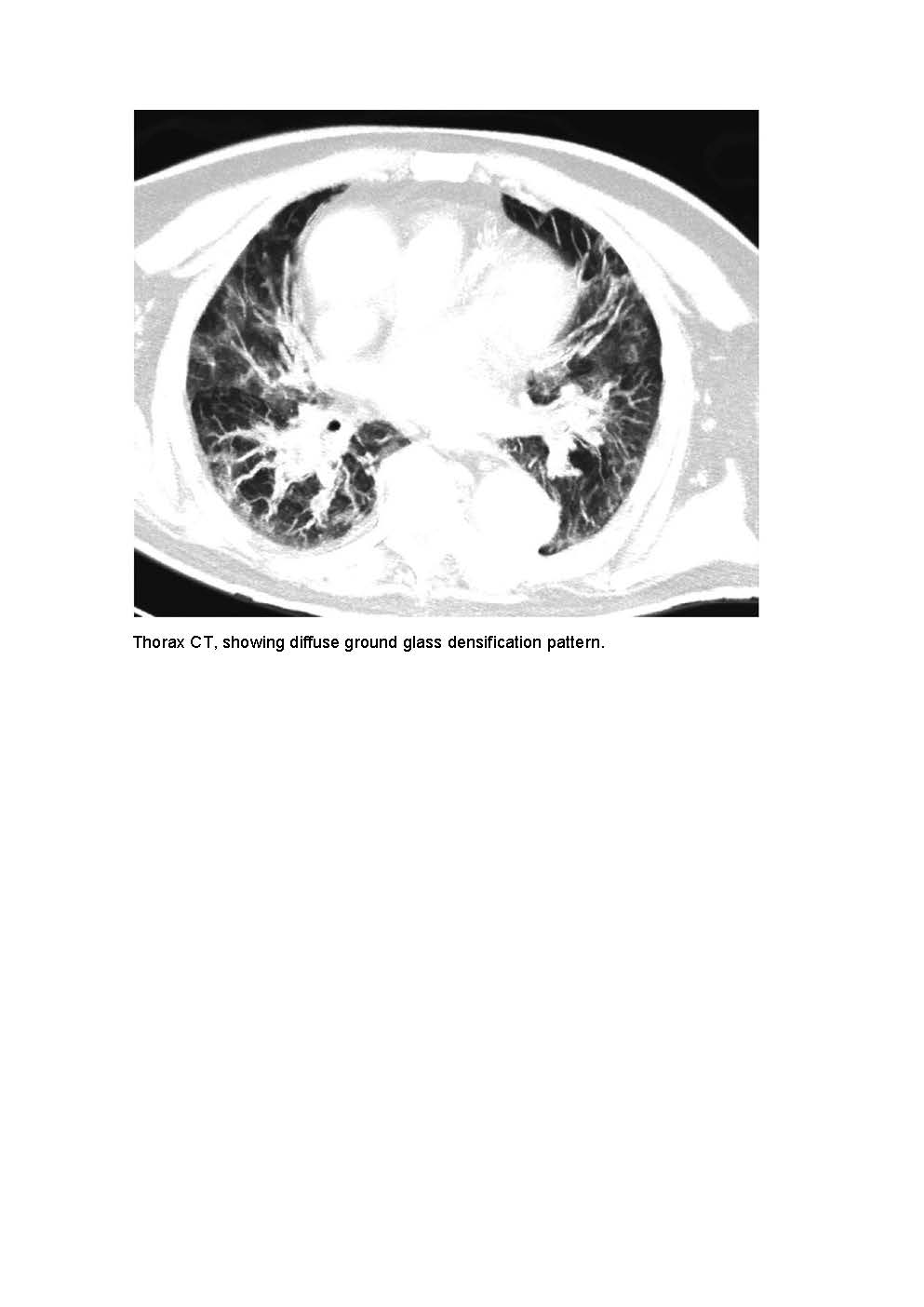
-CoV-2 infection. During hospitalisation he presented with irritability, confusion, fluctuating levels of consciousness and coma. Serology and autoimmunity for neurologic diseases were negative. Electroencephalogram indicated encephalopathy and brain magnetic resonance excluded lesions of inflammatory or vascular nature. A thorax computed tomography scan was performed due to persistent respiratory failure and showed organizing pneumonia. Prednisolone was introduced with neurological and respiratory improvement.
The authors aim to raise awareness for severe COVID-19-
-related encephalopathy and for the fact that, despite having no specific treatment, there is a potential role for high-dose steroids in selected patients. Further studies are needed to understand both the role of steroids and the long-term neurological sequelae of severe COVID-19.
Downloads
References
Ellul MA, Benjamin L, Singh B, Lant S, Michael BD, Easton A, et al. Neurological associations of COVID-19. Lancet Neurol. 2020;19:767-
doi: 10.1016/S1474-4422(20)30221-0.
Uginet M, Breville G, Assal F, Lövblad KO, Vargas MI, Pugin J, et al. COVID-19 encephalopathy: Clinical and neurobiological features. J Med Virol. 2021;93:4374-81. doi: 10.1002/jmv.26973.
Garg RK, Paliwal VK, Gupta A. Encephalopathy in patients with COVID-19: A review. J Med Virol. 2021;93:206-22. doi:10.1002/jmv.26207
Nuzzo D, Vasto S, Scalisi L, Cottone S, Cambula G, Rizzo M, et al. Post-Acute COVID-19 Neurological Syndrome: A New Medical Challenge. J Clin Med. 2021;10:1947. doi: 10.3390/jcm10091947.
Premraj L, Kannapadi NV, Briggs J, Seal SM, Battaglini D, Fanning J, et al. Mid and long-term neurological and neuropsychiatric manifestations of post-COVID-19 syndrome: A meta-analysis. J Neurol Sci. 2022;434:120162. doi: 10.1016/j.jns.2022.120162.
Maury A, Lyoubi A, Peiffer-Smadja N, de Broucker T, Meppiel E. Neurological manifestations associated with SARS-CoV-2 and other coronaviruses: A narrative review for clinicians. Rev Neurol. 2021;177:51-64. doi:10.1016/j.neurol.2020.10.001
Pilotto A, Odolini S, Masciocchi S, Comelli A, Volonghi I, Gazzina S, et al. Steroid-Responsive Encephalitis in Coronavirus Disease 2019. Ann Neurol. 2020;88:423-7. doi: 10.1002/ana.25783.
Venkatesan P. NICE guideline on long COVID. Lancet Respir Med. 2021;9:129. doi: 10.1016/S2213-2600(21)00031-X
World Health Organization. [14th May of 2022] Available at: https://www.who.int/publications/i/item/WHO-2019-nCoVPost_COVID-19_condition-Clinical_case_definition-2021.1
Ceban F, Ling S, Lui LMW, Lee Y, Gill H, Teopiz KM, et al. Fatigue and cognitive impairment in post-COVID-19 syndrome: A systematic review and meta-analysis. Brain Behav Immun. 2022;101:93-135. doi: 10.1016/j.bbi.2021.12.020.
Anaya JM, Rojas M, Salinas ML, Rodríguez Y, Roa G, Lozano M, et al. Post-COVID syndrome. A case series and comprehensive review. Autoimmun Rev. 2021;20:102947. doi: 10.1016/j.autrev.2021.102947.
Yong SJ. Long COVID or post-COVID-19 syndrome: putative pathophysiology, risk factors, and treatments. Infect Dis. 2021;53:737-54. doi:10.1080/23744235.2021.1924397
Downloads
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Ana Rita Ramalho, Adriana Henriques, Helena Rodrigues, Ana Carolina Pires, Inês Gomes, Maja Petrova

This work is licensed under a Creative Commons Attribution 4.0 International License.