Malnutrition: An Underdiagnosed Cause of Wernicke's Syndrome
DOI:
https://doi.org/10.60591/crspmi.95Keywords:
Bariatric Surgery, Malnutrition, Thiamine Deficiency, Wernicke EncephalopathyAbstract
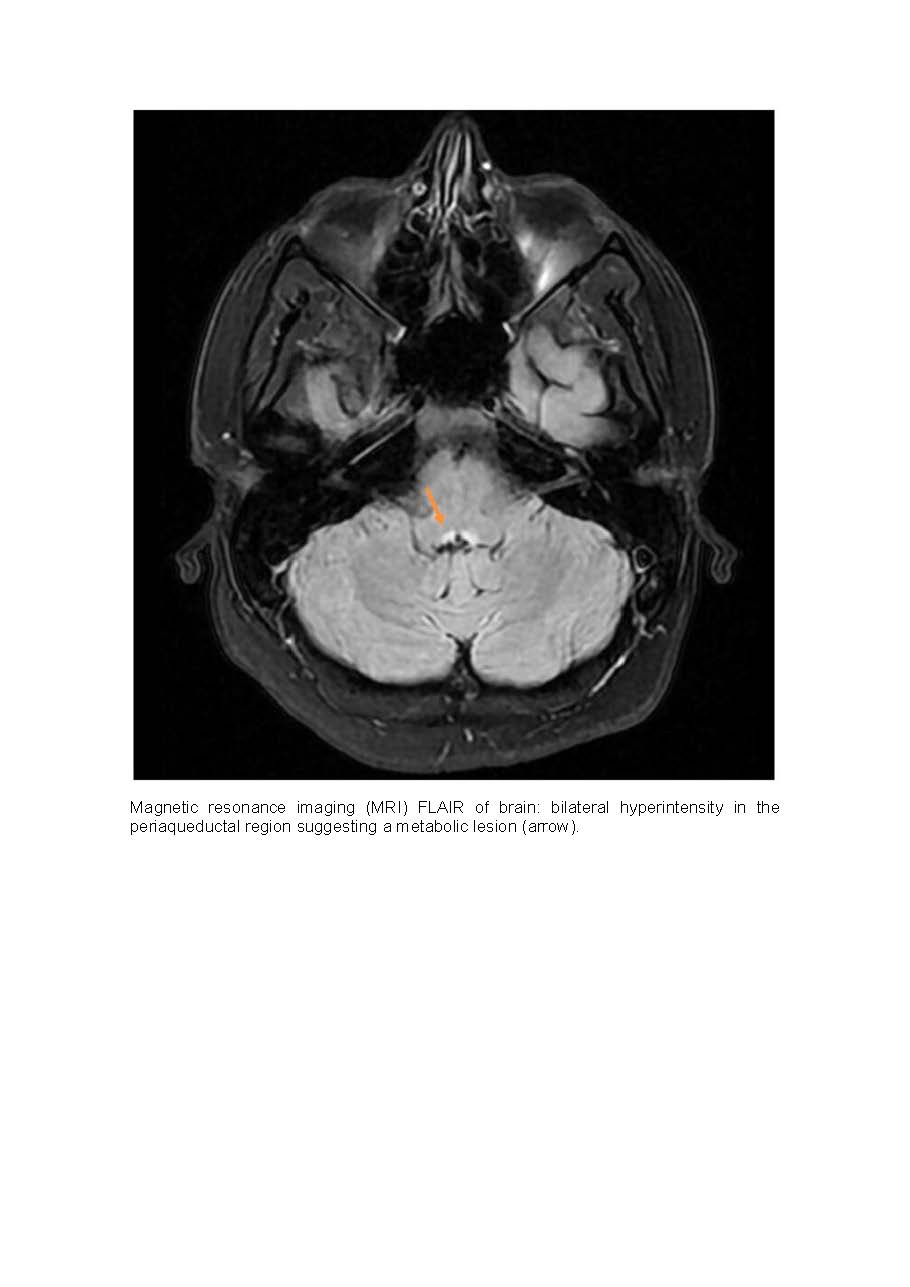
Wernicke syndrome is an underdiagnosed condition, and many cases are not identified in life. The main cause is alcohol abuse, however there are others less evident as malnutrition or bariatric surgery. Generally, this disease
presents with neurological symptoms such as: confusion,
ophthalmoplegia and ataxia. The diagnosis is primarily clinical and often confirmed days later. Magnetic resonance imaging findings are not pathognomonic but can corroborate the diagnosis. Early thiamine treatment is necessary to avoid permanent neurological deficits or even death. We present a case of thiamine deficiency due to malnutrition in an obese patient recently submitted to bariatric surgery. The authors’ purpose is to alert to the importance of maintaining a high level of suspicion for thiamine deficiency, even in patients without history of alcohol abuse for successful outcome.
Downloads
References
Farquet V, Alvarez V, Biselx S, Coutaz M. Du déficit en thiamine à l’encéphalopathie de Gayet-Wernicke, pathologie méconnue. Rev Med Suisse. 2017;13:382–4.
Galvin R, Bråthen G, Ivashynka A, Hillbom M, Tanasescu R, Leone MA; EFNS. EFNS guidelines for diagnosis, therapy and prevention of Wernicke encephalopathy. Eur J Neurol. 2010;17:1408-18. doi: 10.1111/j.1468-1331.2010.03153.x.
Ota Y, Capizzano AA, Moritani T, Naganawa S, Kurokawa R, Srinivasan A. Comprehensive review of Wernicke encephalopathy: pathophysiology, clinical symptoms and imaging findings. Jpn J Radiol. 2020;38:809-820. doi: 10.1007/s11604-020-00989-3.
Javalkar V, Kelley RE, Gonzalez-Toledo E, McGee J, Minagar A. Acute ataxias: differential diagnosis and treatment approach. Neurol Clin. 2014;32:881-91. doi: 10.1016/j.ncl.2014.07.004.
Gasmi A, Bjørklund G, Mujawdiya PK, Semenova Y, Peana M, Dosa A, et al. Micronutrients deficiences in patients after bariatric surgery. Eur J Nutr. 2022;61:55-67. doi: 10.1007/s00394-021-02619-8.
Kröll D, Laimer M, Borbély YM, Laederach K, Candinas D, Nett PC. Wernicke Encephalopathy: a Future Problem Even After Sleeve Gastrectomy? A Systematic Literature Review. Obes Surg. 2016;26:205-12. doi: 10.1007/s11695-015-1927-9.
Yu AT, Gross A, Park K, Harvey EJ. Wernicke Encephalopathy After Bariatric Surgery: a Literature Review. Obes Surg. 2023;33:3621-7. doi: 10.1007/s11695-023-06840-8.
Oudman E, Wijnia JW, van Dam M, Biter LU, Postma A. Preventing Wernicke Encephalopathy After Bariatric Surgery. Obes Surg. 2018;28:2060-68. doi: 10.1007/s11695-018-3262-4.
Downloads
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Diogo Dias, João Barros, Alina Vicas, Mercedes Agúndez, Silvia Lourenço

This work is licensed under a Creative Commons Attribution 4.0 International License.