From Postpartum Hemorrhage to Acquired Hypopituitarism: Clinical Case
Da Hemorragia Pós-Parto ao Hipopituitarismo Adquirido: Caso Clínico
DOI:
https://doi.org/10.60591/crspmi.223Keywords:
Hypopituitarism, Postpartum HemorrhageAbstract
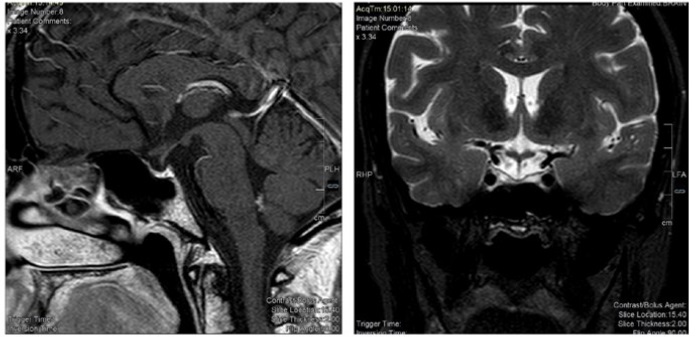
Sheehan’s syndrome is a rare disease associated with hypopituitarism that occurs because of ischemic pituitary necrosis due to severe postpartum hemorrhage. We report a case of a 34-year-old woman with a history of postpartum hemorrhage and subsequent fatigue, weight loss, hair loss, agalactia, amenorrhea, and dyspareunia. Laboratory results revealed microcytic and hypochromic anemia, hypogonadotropic hypogonadism central hypothyroidism, hypoprolactinemia, and adrenal insufficiency. The radiological evaluation helped to establish a definitive diagnosis. This condition, although increasingly less frequent, requires early diagnosis and appropriate treatment to reduce morbidity and mortality.
Downloads
References
Laway BA, Baba MS. Sheehan syndrome. J Pak Med Assoc. 2021;71:1282-12568.
Karaca Z, Laway BA, Dokmetas HS, Atmaca H, Kelestimur F. Sheehan syndrome. Nat Rev Dis Primers. 2016; 2:16092. doi: 10.1038/nrdp.2016.92.
Matsuzaki S, Endo M, Ueda Y, Mimura K, Kakigano A, Egawa-Takata T, et al. A case of acute Sheehan's syndrome and literature review: a rare but life-threatening complication of postpartum hemorrhage. BMC Pregnancy Childbirth. 2017;17:188. doi: 10.1186/s12884-017-1380-y.
Kovacs K. Sheehan syndrome. Lancet. 2003;361:520-2. doi: 10.1016/S0140-6736(03)12490-7.
Laway BA, Sharma A, Choh NA, Shaheen F, Wani AI. Sella turcica size in women with sheehan syndrome-a case-control study. Indian J Endocrinol Metab. 2023;27:431-5. doi: 10.4103/ijem.ijem_316_22.
Kanekar S, Bennett S. Imaging of neurologic conditions in pregnant patients. Radiographics. 2016;36:2102-22. doi: 10.1148/rg.2016150187.
Schury MP, Adigun R. Sheehan Syndrome. 2023 Sep 4. In: StatPearls. Treasure Island: StatPearls Publishing; 2024.
Woodmansee WW. Pituitary Disorders in Pregnancy. Neurol Clin. 2019;37:63-83. doi: 10.1016/j.ncl.2018.09.009.
Genetu A, Anemen Y, Abay S, Bante SA, Mihrete KM. A 45-year-old female patient with Sheehan's syndrome presenting with imminent adrenal crisis: a case report. J Med Case Rep. 2021;15:229. doi: 10.1186/s13256-021-02827-0.
Laway BA, Mir SA, Bashir MI, Bhat JR, Samoon J, Zargar AH. Prevalence of hematological abnormalities in patients with Sheehan's syndrome: response to replacement of glucocorticoids and thyroxine. Pituitary. 2011;14:39-43. doi: 10.1007/s11102-010-0255-2.
Diri H, Karaca Z, Tanriverdi F, Unluhizarci K, Kelestimur F. Sheehan's syndrome: new insights into an old disease. Endocrine. 2016;51:22-31. doi: 10.1007/s12020-015-0726-3.
Downloads
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Joana Gomes da Cunha, Carolina Anjo, Gabriel Atanásio, Vera Romão, Marta Gonçalves Ferreira

This work is licensed under a Creative Commons Attribution 4.0 International License.