Um Caso Raro de Sépsis Fatal por Clostridium perfringens
DOI:
https://doi.org/10.60591/crspmi.347Keywords:
Choque Séptico, Clostridium perfringens, Infeções por Clostridium, SépsisAbstract
Clostridium perfringens é uma bactéria Gram-positiva, comensal da flora gastrointestinal dos seres humanos que pode causar infeções oportunistas como gangrena gasosa e enterocolite necrotizante.
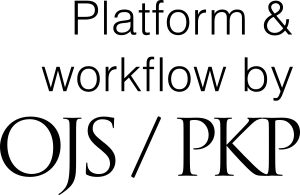
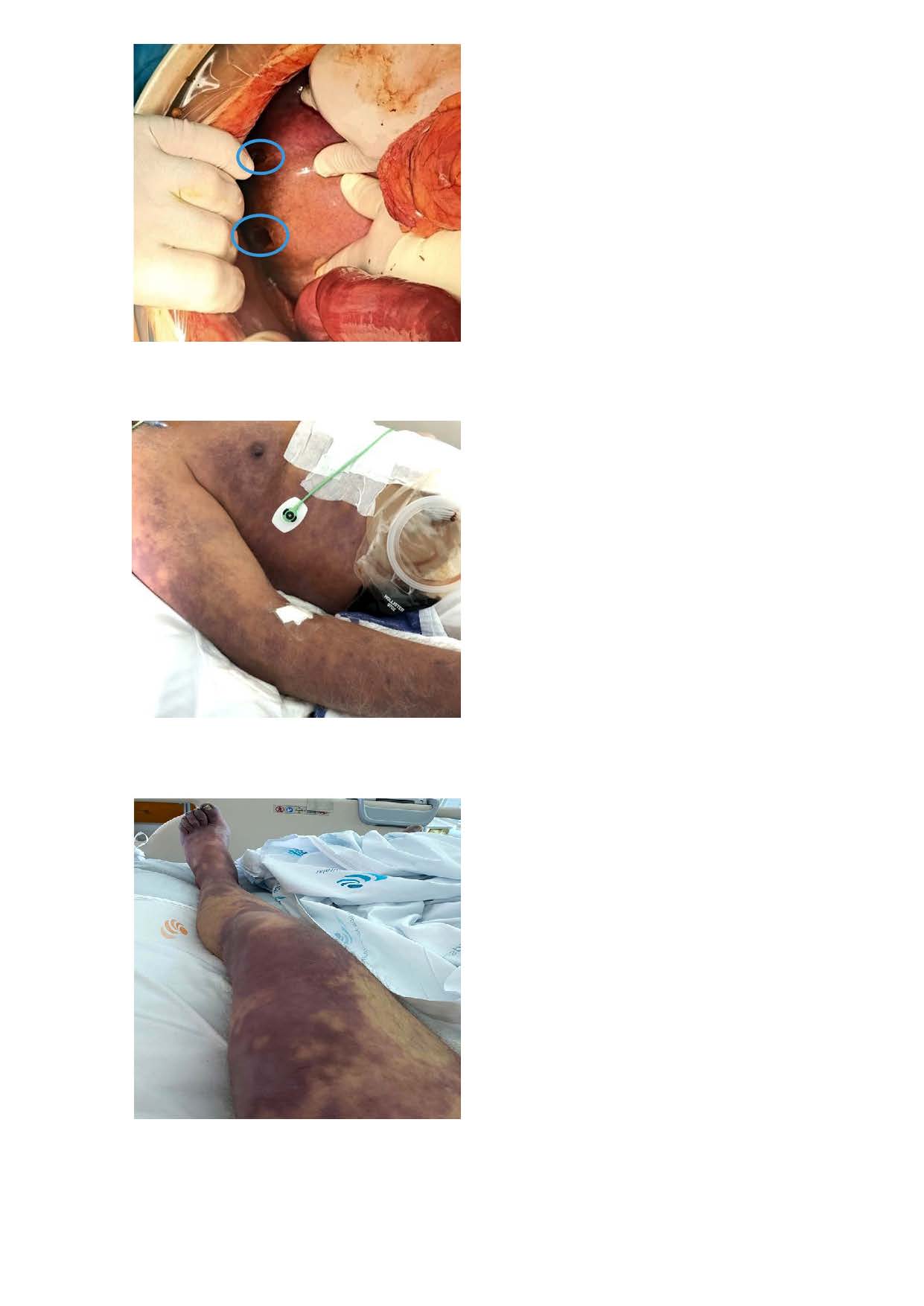
Relatamos o caso de um homem de 71 anos com quadro de dor abdominal e choque séptico com hemólise severa, submetido a laparotomia constatando-se necrose hepática, sinais de má perfusão dos órgãos intra-abdominais e enfisema retal. Apesar do suporte de órgão, apresentou
choque refratário, culminando na morte em 24 horas. Hemoculturas e cultura de líquido peritoneal positivas para Clostridium perfringens.
A bacteriemia por C. perfringens é rara e está associada a altas taxas de mortalidade, podendo chegar a 70%-100% em horas, quando complicada de hemólise, como sucedeu no caso apresentado. Assim, sublinha-se a necessidade de um alto grau de suspeição e intervenção atempada e uma reflexão sobre novas abordagens terapêuticas com vista à diminuição da mortalidade.
Downloads
References
Ohtani K, Shimizu T. Regulation of Toxin Production in Clostridium perfringens. Toxins. 2016;8:207. doi: 10.3390/toxins8070207.
Chinen K. Sudden death caused by Clostridium perfringens sepsis presenting as massive intravascular hemolysis. Autops Case Rep. 2020;10:e2020185. doi: 10.4322/acr.2020.185.
Shibazaki S, Yasumoto T, Nakaizumi T. Massive intravascular haemolysis due to Clostridium perfringens. BMJ Case Rep. 2018;2018:bcr2017223464. doi: 10.1136/bcr-2017-223464.
Shrestha A, Uzal FA, McClane BA. Enterotoxic Clostridia: Clostridium perfringens Enteric Diseases. Microbiol Spectr. 2018;6:10.1128/microbiolspec. gpp3-0003-2017. doi: 10.1128/microbiolspec.GPP3-0003-2017.
van Bunderen CC, Bomers MK, Wesdorp E, Peerbooms P, VeenstraJ. Clostridium perfringens septicaemia with massive intravascular haemolysis: a case report and review of the literature. Neth J Med. 2010;68:343-6.
Hatheway CL. Toxigenic clostridia. Clin Microbiol Rev. 1990;3:66-98. doi: 10.1128/CMR.3.1.66.
Nagahama M, Ochi S, Oda M, Miyamoto K, Takehara M, Kobayashi K. Recent insights into Clostridium perfringens beta-toxin. Toxins. 2015;7:396-406. doi: 10.3390/toxins7020396.
Smith AM, Thomas J, Mostert PJ. Fatal case of Clostridium perfringens enteritis and bacteraemia in South Africa. J Infect Dev Ctries. 2011;5:400-2. doi: 10.3855/jidc.1602.
Fu Y, Alenezi T, Sun X. Clostridium perfringens-Induced Necrotic Diseases: An Overview. Immuno. 2022;2:387-407. doi: 10.3390/immuno2020024
Mishra R, Sinha N, Duncalf R. Beta lactamase producing Clostridium perfringens bacteremia in an elderly man with acute pancreatitis. Case Rep Crit Care. 2016;2016:7078180. doi: 10.1155/2016/7078180.
Shah M, Bishburg E, Baran DA, Chan T. Epidemiology and outcomes of clostridial bacteremia at a tertiary-care institution. ScientificWorldJournal. 2009;9:144-8. doi: 10.1100/tsw.2009.21.
Simon TG, Bradley J, Jones A, Carino G. Massive intravascular hemolysis from Clostridium perfringens septicemia: a review. J Intensive Care Med. 2014;29:327-33. doi: 10.1177/0885066613498043.
Suzaki A, Hayakawa S. Clinical and Microbiological Features of Fulminant Haemolysis Caused by Clostridium perfringens Bacteraemia:Unknown Pathogenesis. Microorganisms. 2023;11:824. doi: 10.3390/ microorganisms11040824.
Takahashi G, Nakamura Y, Hayakawa T, Ono T, Endo K, Yoshida H. Clostridium perfringens sepsis after pancreatoduodenectomy: a case report. Surg Case Rep. 2022;8:48. doi: 10.1186/s40792-022-01402-z.
Wilson PA, Tierney L, Varadhan H. Clostridium Perfringens Infection With Massive Hemolysis. Infect Dis Clin Pract. 2018;26:191-7. doi: 10.1097/IPC.0000000000000630
Fernandez R, Anampa-Guzmán A. Septic Shock Due to Clostridium perfringens. Cureus. 2019;11:e4262. doi: 10.7759/cureus.4262.
Serrano A, Ilustrisimo T, Salvo R, Jeung G, McDermott N. Septic shock due to Clostridium perfringens pyogenic liver abscess: A Rare Infection. Am J Gastroenterol. 2021; 116:S1181. doi: 10.14309/01.ajg.0000784912.89451.19
Kohya R, Murai T, Taguchi Y, Sawai K, Takehara M, Nagahama M, et al. An Autopsy Case of Rapidly Aggravated Clostridium perfringens Septicemia with Colorectal Cancer. Case Rep Infect Dis. 2022:30;2022:1071582. doi: 10.1155/2022/1071582.
Rajendran G, Bothma P, Brodbeck A. Intravascular haemolysis and septicaemia due to Clostridium perfringens liver abscess. Anaesth Intensive Care. 2010;38:942-5. doi: 10.1177/0310057X1003800522.
Downloads
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2025 Cátia Gorgulho, Joana Freitas Ribeiro, Débora Lopes, Luís França, Nuno Catorze

This work is licensed under a Creative Commons Attribution 4.0 International License.